Implanting even a large skull section may seem like a relatively small victory in the dramatic context of the ongoing war but it’s making a huge difference in this soldier’s life.
Last year a surgical team led by retired Air Force Col. (Dr.) Warren Dorlac, a Uniformed Services University alumnus and Associate Professor of Surgery, arrived in Ukraine, to begin a volunteer mission supporting Ukraine’s civilian Emergency Medical Clinical Hospital. Dorlac, a recognized expert in trauma surgery and trauma care, was uniquely qualified to lead the team. After a few months of activity in Ukraine, when faced with the case of a Ukrainian soldier who had lost a large part of his skull, he immediately knew that no existing implant solution could address this type of injury. So, he contacted a well-known US-based institute for regenerative medicine and, through them, got in touch with bioprinting specialist T&R Biofab, with the goal to create a unique, resorbable PSI.
“As a military surgeon, I have seen the worst that humanity can do, but I have also been fortunate enough to see the best,” said Dorlac, writing from Lviv to its Alma Mater, USU. “It is a privilege to be part of this lifesaving mission serving the brave people of Ukraine.”
Bringing out the best
This unique collaboration with T&R falls under the “best” category. Not only did it help the Ukrainian soldier fully recover from an injury that would have been completely debilitating or worse, but it also showed how useful additive manufacturing can be when no other solution exists. The section of the skull that needed to be replaced was larger than any implant readily available, especially considering that metal is not usually a feasible solution for such a large part of the skull. In addition, it needed to be personalized to achieve an ideal fit.
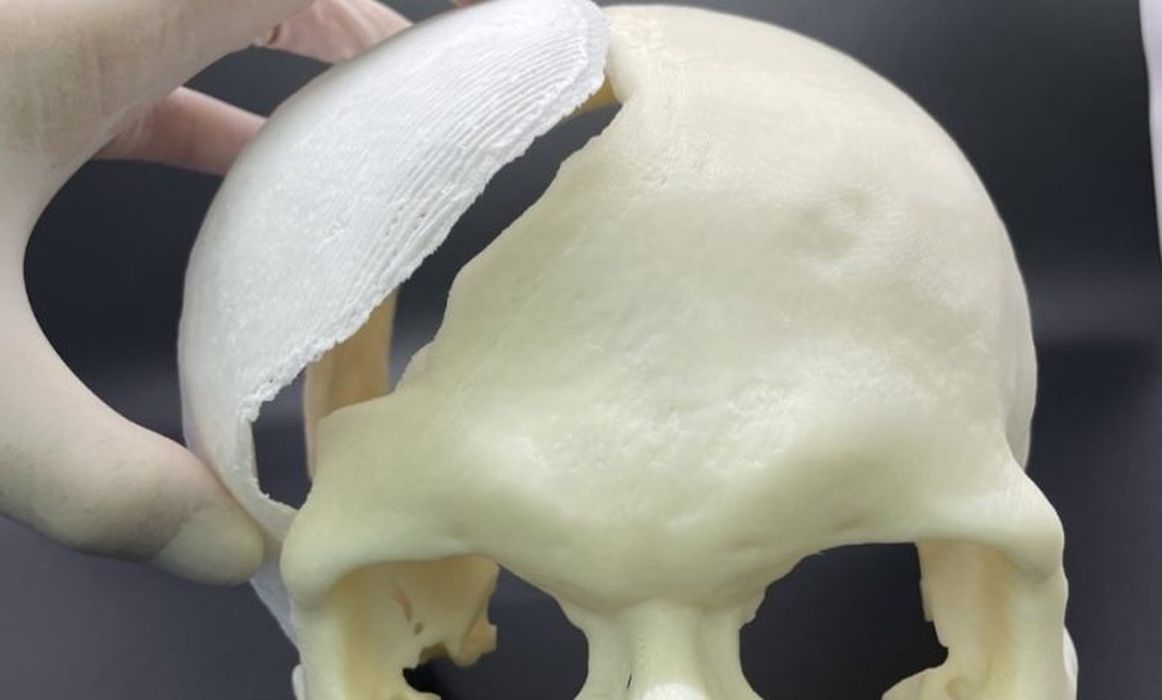
That’s why T&R’s technology provided the only possible solution: its 3D bioprinters can print using various biomaterials, including deCelluid (a hydrogel tissue-derived bioink), ceramics as well as synthetic and biodegradable (bioresorbable) polymers that can ideally replicate special tissue microenvironments through the printing process. In this case the PCL : TCP material, a mixture of bioresorbable polycaprolactone (PCL) and beta-tricalcium phosphate (which is one of the materials human bones are made of) provided the ideal environment for a skull implant that would be strong enough and that would enable the bone to grow back onto and into it.
Within their first few days in Ukraine, Dorlac’s evaluated conditions, offered recommendations and delivered lectures and training on topics including end points of resuscitation and the use of ultrasound in trauma and critical care. According to Dorlac, emergency medicine is not a dedicated specialty in Ukraine. The emergency hospital staff that the team assisted included trauma and general surgeons, thoracic surgeons, vascular surgeons, pediatric surgeons, orthopedic surgeons, anesthesiologists/intensivists, and surgical and critical care nurses. The caseload included “typical combat wounds –- extensive burns, complex fractures, nerve injuries, soft tissue loss, and wounds and amputations,” said Dorlac.
Dorlac was accompanied on the Ukraine mission by a distinguished team of medical professionals including military trauma surgeon and USU Surgery department faculty member Air Force Col. (Dr.) Jay Johannigman, renowned burn surgeon Dr. William Hickerson, and surgical physician assistant Kelley Thompson. With their work in Ukraine, Dorlac, Johannigman and the other surgical team members continue the tradition of US military medical aid for conflict victims around the world, a tradition interwoven throughout USU’s entire 50-year history, beginning with Dr. Rich.
Emergency lifesaving solutions
To design and produce the proper PSI, multiple meetings had to be held between T&R Biofab, the Ukrainian surgeons and US doctors. Once the exact specifications required were ascertained, T&R manufactured the implant within days, based on the CT data that was sent to the company directly from Ukraine. At this point the T&R team used its bioprinting technology to produce 3 identical custom cranial implants. These were then shipped out to Poland so that they could be delivered by military personnel to the surgeons operating inside Ukraine.
The first of the three PSIs was immediately used for the intended patient. During the operation, US and Ukrainian doctors shared knowledge on how to use the implant through online meetings and the surgery was a complete success. The surgeons confirmed that the results were very satisfactory and pointed out that it was easier to operate since the PSI fit so well with the actual defect in the skull. The patient has since been recovering without complications.
Read the rest of this story at VoxelMatters
