Though found in different areas of the animal kingdom, the degree to which humans can regenerate limbs, organs and tissue due to serious injury is very low (one exception is the liver), especially compared to animals like the amazing Axolotl. Scientific research into using 3D bioprinting to re-create and regenerate human limbs and organs from patient-specific DNA is progressing slowly but surely.
The implications and potential for organ transplant patients with life-threatening prognoses is profound. Even when there is an organ donor match for patients in need of a transplant, rejection by the host of the transplanted organ is a constant threat to completed surgery. Organ transplant patients undergo rejection prophylaxis, which involves taking a suite of medicines for the purpose of preventing or reducing organ rejection. If surgeons and medical professionals could offer patients a “copy” of their organs based on their own DNA profiles, rejection prophylaxis could become unnecessary.
Architects have a great difficulty recreating the geometry of old buildings using 3D scanning. The geometry of manmade structures from years past are far different than in-built geometry of 3D design software that is used to create new building designs. Scanning naturally occurring geometry is relatively advanced now, but replicating naturally occurring geometry is problematic in many areas. The geometry is vastly more complex than anything produced by 3D software, and the same is true of the biological structures that make up the hyper-complicated universe that is human anatomy.
Bioprinting Aortic Valve (Department of Bioengineering at the University of Cornell)
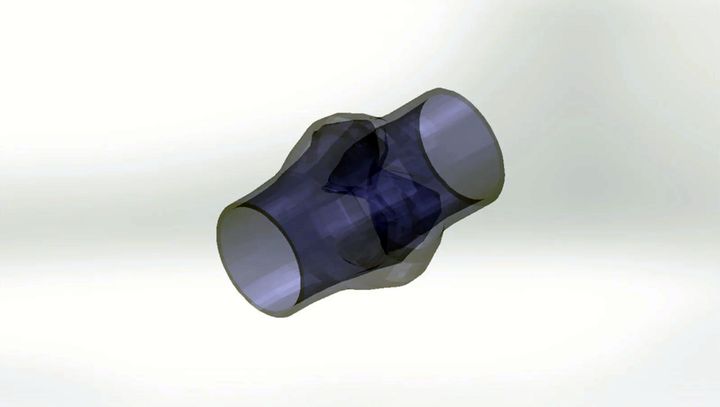
At Cornell University, a group of researchers are exploring and experimenting with printing a human aortic valve for aortic valve replacement surgery. The researchers know that the aortic valve has the complex geometry needed for efficient biomechanical function. As with most naturally occurring geometry, the researchers can get a comprehensive scan and 3D model of aortic valves. A far more difficult task is to recreate the living biological tissue and ensure that it is similar enough to naturally occurring aortic valves so that the bioprinted valves can be used for surgery. The physical world is far more finicky to replicate with near-perfect accuracy.
Using a new “simultaneous 3D printing with controlled photocrosslinking technique,” Cornell researchers were able to 3D print complex aortic valve scaffolds, which ranged from 12-22mm in inner diameter, from poly-ethylene glycol-diacrylate (PEG-DA) hydrogels supplemented with alginate. After printing these scaffolds, their geometry was captured by micro-computed tomography scans and cultured for 21 days. They were tested to compare rates of bioelasticity. The prints were achieved in 14-15 minutes.
Overall, the results showed that 3D hydrogel printing with controlled photocrosslinking can rapidly create anatomically correct valve conduits that would support living cell grafts. In other words, the scaffolding of a “living” structure can be rapidly bioprinted and living cells can grow into an aortic valve from them.
Bioprinting Microtia Reconstruction
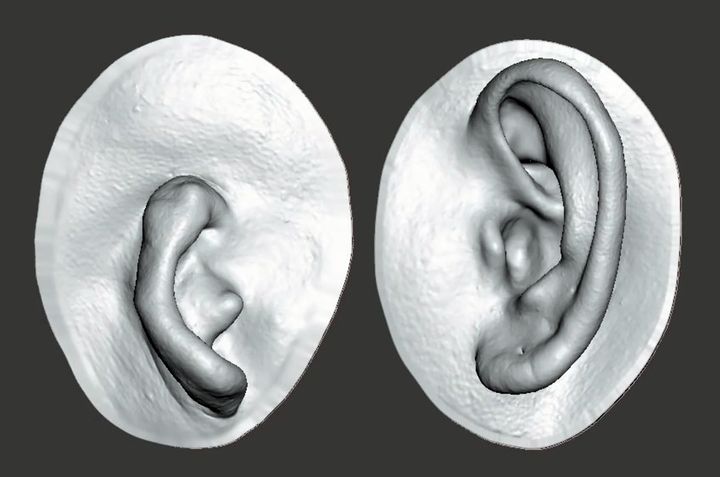
Microtia is a deformity present from birth where the pinna (external ear) is underdeveloped. Researchers from the College of Engineering at the Swansea University in the UK published a 2016 paper entitled, “Could 3D bioprinted tissues offer future hope for microtia treatment?” The paper described the difficulties facing patients with microtia. Microtia reconstruction is a high-risk surgery, but stem cell-based bioprinting could offer solutions to microtia patients and others with tissue abnormalities. The paper mentions ongoing research to produce cartilage tissues for reconstructive surgery using bioprinting. The technique described is like the more recent research performed by Cornell University on aortic valves.
Read more at ENGINEERING.com
