![The 3D printed gas exchange component of a future artificial lung [Source: U.S. Department of Veterans Affairs]](https://fabbaloo.com/wp-content/uploads/2020/05/va-bioprinted-lung-ov_result_img_5eb0a8d08932a.jpg)
Researchers at the U.S. Department of Veterans Affairs (VA) are developing a 3D printed lung, with some interesting implications.
They’re trying to solve or at least assist in the handling of veterans suffering from COPD, or chronic obstructive pulmonary disease. This is an affliction in which active lung tissue gradually becomes ineffective, leading to shortness of breath or coughing, with an associated reduction of individual activity.
While the general public can acquire COPD through tobacco smoking or exposure to air pollution, veterans in active conflicts can encounter situations where they are exposed to pollutants or toxic gases that also cause COPD.
The goal of the research project is to develop an artificial lung system that can handle some of the overflow work unable to be accomplished by a COPD-afflicted set of lungs. Typically this would be done while awaiting a transplant or other rectifying procedure.
The artificial lung would act in much the same way as a real lung: blood would be exposed to a gas-transfer surface where oxygen can make the jump from the atmosphere to hemoglobin. But the implication of this in a mechanical sense is that blood would be in contact with potentially toxic machinery, where natural body immune systems might view it as a foreign object (which it is) and react negatively.
![Another view of the 3D printed gas exchange component of a future artificial lung [Source: U.S. Department of Veterans Affairs]](https://fabbaloo.com/wp-content/uploads/2020/05/image-asset_img_5eb0a8d0e2d8e.jpg)
Artificial lungs exist today, but they are essentially bulky machines requiring considerable resources and their size effectively prevents the user from being mobile. One of the goals here would be to develop a system that’s sufficiently compact to enable development of a truly portable – and even wearable – artificial lung.
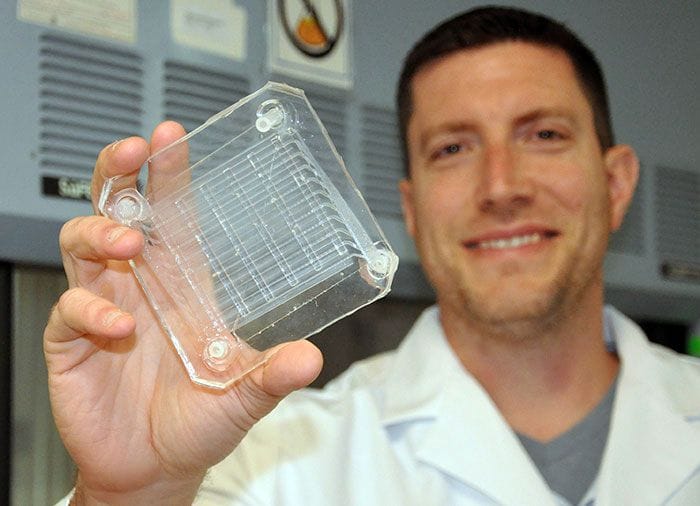
Most of the lung design would be straightforward, with tubing, attachments, pumps, etc., with the key element being the component where the actual gas business takes place: the gas exchange filter.
This structure would be similar in design to a radiator, where the fluid (blood) is spread across a vast array of small channels to maximize the surface area exposure to the gas transfer layer.
In this project, it’s done by 3D printing a tiny microfluidic structure that contains viable vessels to carry the blood through.
As you can imagine, other approaches for developing such a structure would be challenging, whereas 3D printing can, as usual, create virtually any arbitrary structure.
The catch here is that the microfluidic structure must contain very, very small elements – and be biocompatible at the same time.
The VA is working with Old World Laboratories, a company we’ve spoken to in the past. I recall they were the company that showed us what was probably the smallest 3D print I’ve ever seen in person. In fact, it was so small I could not really see it. They would be an obvious choice for such finely detailed work.
![Very tiny 3D printed samples made by Old World Laboratories [Source: Fabbaloo]](https://fabbaloo.com/wp-content/uploads/2020/05/image-asset_img_5eb0a8d15791e.jpg)
One of their challenges in 3D printing this object is the need to apply a biocompatible coating. I’m not sure if they are 3D printing it or applying it to the print afterwards, which is a more likely approach, come to think about it.
It’s not clear whether the project will succeed, but if it does this would be considered a milestone in bioprinting: most bioprinting today is of “solid” or “flat” structures such as skin. The problem often encountered is that 3D printed tissue tends to die off because there are no vessels to deliver nutrients to the tissue, and any nutrients must “soak in” from the outside surface.
But the VA project’s outcome might have a side effect: the ability to 3D print biocompatible tissue with embedded blood vessels. This capability could open up many possibilities for 3D printed tissues that up to now have been difficult to develop.
Via U.S. Department of Veterans Affairs










FELIXprinters has released a new bioprinter, the FELIX BIOprinter, which is quite a change for the long-time 3D printer manufacturer.